|
|
|||||||||||||||||||||
|
|
|||||||||||||||||||||
|
Toward
an Evidence-Informed |
|||||||||||||||||||||
|
Author:
Madeline Roberts, PhD, MPH Interestingly, no standard definition exists for a chronic condition. The U.S. Department of Health and Human Services (HHS), the U.S. National Center for Health Statistics, and peer-reviewed literature all differ in their definitions of chronic disease, which has implications for reporting and surveillance efforts. The definitions differ on integral points such as duration, functional limitations, and the need for ongoing medical care. A non-exhaustive list of conditions eligible for CMS chronic care management services includes hypertension, HIV, osteoporosis, and substance use disorders, among others.
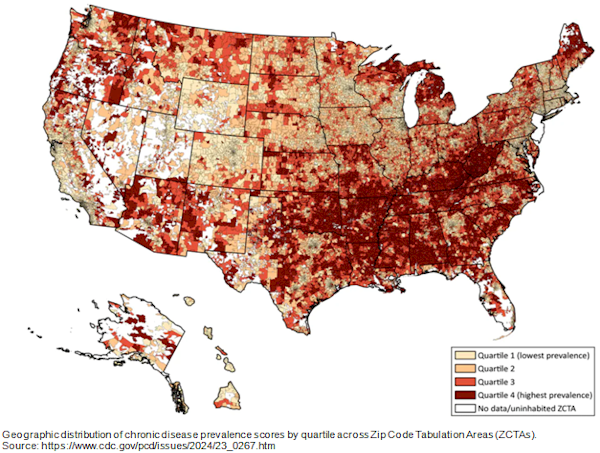
Interesting recent evidence exists on specific age intervention points and modifiable risk factors for chronic conditions. Molecular changes associated with aging appear to follow a nonlinear pattern, with disproportionately higher decline occurring around ages 44 and 60. ♦ Around age 40 to 44, the body becomes less efficient at metabolizing fat; the same appears true for alcohol and caffeine. Cardiovascular disease risk increases. ♦ Around age 60, the body becomes less efficient at carbohydrate metabolization, and there is a decline in the immune system and kidney function. The risk for cardiovascular disease, kidney disease, and type 2 diabetes markedly increases. Identifying molecular dysregulation and decline at these specific age points is powerful for informing population health screenings and clinical preventive measures. Environmental exposures impact disease patterns and premature mortality more than genetics in many cases, according to a recent UK study. Primary drivers of mortality and aging included smoking, hours of sleep, household income, home ownership, ethnicity, years of education, physical activity and wellness, and the additive effect of these factors together. This emphasizes the utility of environmental interventions in mitigating premature mortality, as nearly all of these factors are modifiable. Non-modifiable factors were height (shorter is somewhat protective) and ethnicity. Additionally, genetic risk contributed more than environmental factors in the development of dementia and breast, prostate, and colorectal cancers. Conversely, environmental factors contributed more than genetics in the development of diseases of the heart, lungs, and liver. The recent “Ten Americas” study defined ten different Americas based on race, ethnicity, location, metropolitan status, income, and Black–White residential segregation. It showed dramatic differences in U.S. life expectancies by subpopulation. Life expectancy is less than 64 years for Native Americans living in the western US. By contrast, Asian individuals in the US have a life expectancy of approximately 84 years. Substantial differences in income and education among the ten Americas were also identified. This study provides bleak, quantifiable evidence of the colossal differences in subsets of the US population and demonstrates the severity of the need for tailored population health interventions in areas such as nutrition, substance use, and hypertension. Bottom line: Prevalence data, life expectancy, and epigenetic studies all indicate the need for demographically and geographically tailored interventions rather than a top-down, one-size-fits-all approach for chronic conditions. State and territorial public health departments got hammered during the pandemic and are struggling to regroup, but their work remains indispensable, maybe even more so for chronic conditions. Health workers who are fluent in the unique needs and risk factors of their communities are essential to alleviating the burden of chronic conditions. ■ |
|||||||||||||||||||||
|
|
|||||||||||||||||||||